Definition
Childbirth is formally divided by the medical field into three stages. The first stage is labor, which has three phases: early, active, and transitional. The first stage ends with complete dilatation (opening) of the cervix. The second stage is delivery, which involves pushing and the actual birth of the baby. The third stage is delivery of the placenta or afterbirth.
DescriptionA full-term pregnancy is considered to be 280 days, nine calendar months or ten lunar months calculated from the first day of the last menstrual period. This is a fairly arbitrary number that may, in fact, vary with genetic differences and depends on a normal menstrual cycle, which varies considerably from woman to woman. The average actual length from conception to birth is estimated as 267 days. Childbirth is a natural process,
 Childbirth in stage 2. The baby's head is crowning and about to emerge from the vagina.
Childbirth in stage 2. The baby's head is crowning and about to emerge from the vagina.(Illustration by Hans & Cassidy.)
and it, too, varies among women. Despite what the obstetrical texts say about what to expect, there are many variations that make each woman's experience hers alone. The whole process averages about 14 hours for first-time mothers and about eight hours for mothers in their subsequent pregnancies.
Labor can be described in terms of a series of stages.
First stage of laborDuring the first stage of labor, the cervix dilates (opens) from 0 to 10 centimeters (cm). This stage has an early, or latent, phase, an active phase, and a transitional phase. The latent phase usually lasts the longest and is the least intense phase of labor. This phase is characterized by dilatation (opening) of the cervix to 3–4 cm along with the thinning out of the cervix (effacement). It can take place over a period of days without being noticed or over a period of two to six hours with distinctive contractions. Most women are relatively comfortable during the latent phase, and walking around is encouraged, since it naturally stimulates the process.
With the initiation of labor, the muscular wall of the uterus begins to contract causing the cervix to open (dilatation) and thin out (efface). For a first-time mother the cervix must completely efface before dilatation continues. Effacement is reported in percentages as 50 percent or 100 percent, which is completely thinned out. The amniotic sac may or may not break during labor, and the birth attendant may rupture the bag with an amnio-hook, which looks a little like a large crochet hook. There is no pain involved with the breaking the bag of waters, although the contractions may intensify. During a contraction, the infant experiences pressure that pushes it against the cervix to assist with the dilatation. During this first phase, a woman's contractions typically increase in frequency and duration. Periodic vaginal exams are performed by the physician or nurse to determine progress. As pain and discomfort increase, however, the woman may be tempted to request pain medication. The administration of pain medication or anesthetics should be delayed until the active phase of labor begins, at which point the medication will not act to slow down or stop the labor.
The active phase of labor is usually shorter than the first, lasting an average of two to four hours. The contractions are more intense and accomplishing more in less time. They may be three to four minutes apart lasting 40–60 seconds even though the pattern may not be regular. During the active phase, dilatation continues to 7 cm. Relaxing between contractions is essential for coping because these contractions are more intense. Breathing exercises learned in childbirth classes can help the woman cope with the discomfort experienced during this phase. Pain medication offered at this point consists of either a short-term medication, such as Nubain or Stadol, or long-term such as epidural anesthesia.
The transitional phase continues dilation 7–10 cm. It is the most exhausting and demanding phase of labor. The contractions become very strong, are two to three minutes apart, and last 60–90 seconds. It may feel as if the contractions never stop, and there is no time to relax between them. Dilatation of the final 3 cm to 10 cm takes, on average, 15 minutes to an hour. Strong rectal pressure, with or without an urge to push or move the bowels, may cause the woman to grunt involuntarily. If it is a natural labor and delivery, the laboring woman at this phase becomes very inwardly focused and can lose control. It is important to breathe with her through contractions as this keeps her attention on what she needs to do.
Second stage of laborUp to this point, the woman may feels as if her participation is small, because all she has done is breathe. Active involvement can now begin along with some emotional relief that it is almost over. Without anesthesia, there is often an overwhelming urge to push, and the mother gets a second wind. The baby's head is through the cervix and on its way down the birth canal. The uterine contractions get stronger, and the infant passes along the vagina helped by contractions of the uterus and the mother's pushing. If an epidural anesthetic is being used, many practitioners recommend decreasing the dosage so the mother has better control of her pushing. Research has shown, however, that the contractions will continue to push the baby down the birth canal without mother's help. If a woman is numb from an epidural, she cannot push effectively, and it is usually better to let the contractions work alone. This is called "laboring down."
When the top of the baby's head appears at the opening of the vagina, the birth is nearing completion. First
 A newborn baby sits crying on the mother's stomach.
A newborn baby sits crying on the mother's stomach.(© Jules Perrier/Corbis.)
the head passes under the pubic bone. It fills the lower vagina and stretches the perineum (the tissues between the vagina and the rectum). This position is called "crowning," since only the crown of the head is visible. When the entire head is out, the shoulders follow. The attending practitioner suctions the baby's mouth and nose to ease the baby's first breath. The rest of the baby usually slips out easily, and the umbilical cord is cut.
EpisiotomyMany practitioners argue that it is better to cut the perineum than to let it tear. This cut is called an episiotomy. In reality, it is more difficult to repair a straight cut than a small tear in much the same way it is harder to put together a puzzle with straight edges; it is more difficult to match evenly and can result in vaginal discomfort once healed. Instead, the perineum can be massaged and gently stretched to prevent tearing as the baby's head crowns. There is also less pain associated with a tear than an episiotomy. If the woman has not had an epidural or pudendal block, she will get a local anesthetic to numb the area for repair.
Third stageIn the final stage of labor, the placenta is expelled by the continuing uterine contractions. The placenta is pancake shaped and about 10 cm (25 cm) in diameter. During pregnancy, it is attached to the wall of the uterus and served to exchange needed nourishment from the mother to the fetus and simultaneously to remove waste products from the fetus. Generally, there is a rise in the uterus due to a contraction and a gush of blood as the placenta is expelled. The placenta should be examined to make sure it is intact. Retained placenta can cause severe uterine bleeding after delivery, and it must be removed.
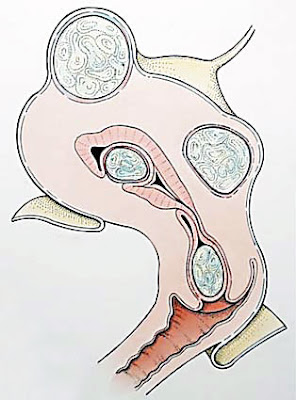
Breech presentationApproximately 4 percent of babies present in the breech position when labor begins. In this presentation, the baby's bottom is the presenting part instead of the head, which is called a vertex presentation. Using a technique called a version, an obstetrician may attempt to turn the baby to a head down position. This is only successful approximately half the time, and there are possible complications with the procedure, such as umbilical cord entanglement and separation of the placenta. However, some practitioners are very successful with versions, and it does make a vaginal delivery safer.
The risks of vaginal delivery with breech presentation are much higher than with a head-first (vertex) presentation. The mother and attending practitioner need to weigh the risks to make a decision on whether to deliver via a cesarean section or attempt a vaginal birth. The degree of risk depends to a great extent on which one of the three types of breech presentations it is. In a frank breech the baby's legs are folded up against its body. This is the most common breech presentation and the safest for vaginal delivery. The others include complete breech, in which the baby's legs are crossed under and in front of the body, and footling breech, in which one leg or both legs are positioned to enter the birth canal. Neither of these is considered safe enough for a vaginal delivery.
Even with a complete breech, there are other factors to consider for a vaginal birth. An ultrasound examination should be done to determine that the baby's head is not too large and that it is tilted forward (flexed) rather than back (hyperextended). Fetal monitoring and close observation of the progress of labor are also important. A slowing of labor or any indication of difficulty in the body passing through the pelvis should be an indication that it is safer to consider a cesarean section.
Forceps deliveryAlthough not used as much in the early 2000s as in earlier times, forceps can be used if the baby's head is very low in the birth canal. Also, if there is some sudden change in the maternal-fetal status, the doctor may opt for a forceps delivery if it would be faster than a cesarean section. Forceps are spoon-shaped devices that can be placed around the baby's head while the doctor gently pulls the baby out of the vagina.
Before placing the forceps around the baby's head, pain medication or anesthesia may be given to the mother. The doctor may use a catheter to empty the mother's bladder and may clean the perineal area with soapy water. Often an episiotomy is done before a forceps birth, although tears can still occur. The use of forceps can cause vaginal lacerations in the mother.
Half of the forceps are slid into the vagina and around the side of the baby's head to gently grasp the head. When both forceps are in place, the doctor pulls on them to help the baby through the birth canal during a uterine contraction. The frequency of forceps delivery varies from one hospital to the next, depending on the experience of staff and the types of anesthesia offered at the hospital. Some obstetricians accept the need for a forceps delivery as a way to avoid cesarean birth while other obstetrical services do not use forceps at all. Complications from forceps deliveries can occur, such as nerve damage or temporary bruises to the baby's face. When used by an experienced physician, forceps can save the life of a baby in distress.
Vacuum-assisted birthThis method of delivering a baby was developed as a gentler alternative to forceps. Similar to forceps deliveries, vacuum-assisted births can only be used with a fully dilated cervix and a well-descended head. In this procedure, a device called a vacuum extractor is used by placing a large rubber or plastic cup against the baby's head. A pump then creates suction that gently pulls on the cup to ease the baby out the birth canal. The force of the suction may cause a bruise or swelling on the baby's head, but it resolves in a day or two.
The vacuum extractor is less likely to injure the mother than forceps, and it allows more space for the baby to pass through the pelvis. There can be problems in maintaining the suction during the vacuum-assisted birth, however, so forceps might be a better choice if the delivery needs to be expedited.
Cesarean sectionsA cesarean section, also called a c-section, is a surgical procedure in which an incision is made through a woman's abdomen and uterus to deliver her baby. This procedure is performed whenever abnormal conditions complicate labor and vaginal delivery that threaten the life or health of the mother or the baby. The procedure is performed in the United States on nearly one in every four women resulting in more than 900,000 babies each year being delivered by c-section. The procedure is often used in women who have had a previous c-section, but if the incision on the uterus is not vertical, the woman can try a vaginal birth after cesarean (VBAC).
Dysfunctional labor is commonly caused by one of the three following conditions: maternal structural abnormalities; abnormal fetal presentations; failure to progress. Non-reassuring fetal heart rate tracings represent a condition in which the fetus may not be tolerating labor and oxygen deprivation can occur. Other conditions which might indicate a need for c-section include: vaginal herpes, hypertension (high blood pressure), and uncontrolled diabetes in the mother.
Causes and symptomsChildbirth usually begins spontaneously, but it may be started by artificial means if the pregnancy continues past 41 weeks gestation. There are three signs that labor may be starting: rhythmical contractions of the uterus; leaking of the bag of waters (amniotic sac); and bloody show. The importance of the sign of contractions is in the rhythm and not the contractions. True labor contractions may start once every ten or 15 minutes or even at longer intervals, but gradually the interval decreases until they come every three to four minutes. The most important thing a woman can do at this phase is to remain relaxed. The bag of waters may leak slowly or may suddenly burst, and there is a gush of fluid. There is no pain when the water breaks, although it may be startling. If contractions are not ongoing prior to this, they are likely to start soon after. If they do not, it may be necessary to stimulate labor as the womb is now open to possible infection. The bloody show is a slight discharge of blood and mucus. It usually occurs after the cervix has started to dilate slightly and the mucus plug that keeps the cervix sealed from potential pathogens becomes dislodged.
DiagnosisThe diagnosis of true labor can only be determined by a vaginal exam to determine if the cervix has changed in dilatation (opening). True labor is determined by whether the contractions are, in fact, changing the cervix. If a woman is experiencing contractions and makes no cervical change, then this is false labor. Dilatation is measured in centimeters and it goes from zero to ten centimeters, which is complete dilatation. Although the woman having the contractions may feel like she is really experiencing labor, true labor is determined by cervical change. Many women may experience Braxton-Hicks contractions (practice contractions) in preparation for true labor, and these can become uncomfortable at times, which prevents the woman from resting. A warm bath or warm drink may help her to relax and sleep. Inevitably she will wake up in true labor with effective contractions. Palpating contractions as they occur can assist in determining whether they are strong. A very strong contraction cannot be indented and will feel as hard as the forehead. A moderate contraction will palpate like the feel of the chin and an easy contraction feels like the end of the nose. If the contractions can be indented, they probably do not constitute true labor.
Electronic fetal monitoringElectronic fetal monitoring (EFM) involves the use of an electronic fetal heart rate (FHR) monitor to record the baby's heart rate. The FHR is picked up by means of an ultrasound transducer and the movement of the heart valves. Elastic belts are used to hold sensors against the pregnant woman's abdomen. The sensors are connected to the monitor and detect the baby's heart rate as well as the uterine contractions. The monitor then records the FHR and the contractions as a pattern on a strip of paper, called a tracing. Electronic fetal monitoring is frequently used during labor to assess fetal well-being. EFM can be used either externally or internally. Internal monitoring does not use ultrasound, is more accurate than electronic monitoring, and provides continuous monitoring for the high-risk mother. An internal monitor requires that the bag of waters be broken and that the woman is at least two to three centimeters dilated. It is used in high-risk situations or when it is difficult to obtain an accurate FHR tracing.
Telemetry monitoring has been available since the early 1990s but is not used in many hospitals as of 2004. Telemetry uses radio waves transmitted from an instrument on the mother's thigh, which allows the mother to remain mobile. It provides continuous monitoring and does not require the patient to be in bed continuously.
Besides EFM and telemetry, which is usually continuous, there is intermittent monitoring using a hand-held Doppler to assess the FHR. This method gives the mother freedom of movement during labor. Prior to electronic gadgetry a special stethoscope was used, called a fetoscope, which is rarely seen as of 2004 because it requires more skill to use. Research on the use of intermittent monitoring and continuous monitoring found no difference in fetal outcomes with intermittent monitoring. The use of continuous monitoring does result in a higher c-section rate partly because the tracing can be misinterpreted or because the mother usually requires more interventions when she cannot be mobile.
TreatmentMany women choose some type of pain relief during childbirth, ranging from relaxation and imagery to drugs. The specific choice may depend on what is available, the woman's preferences, her doctor's recommendations, and how the labor is proceeding. All drugs have some risks and some advantages.
Regional anestheticsRegional anesthetics include epidurals and spinals. With this procedure, medication is injected into the space surrounding the spinal nerves. Depending on the type of medications used, this type of anesthesia can block nerve signals, causing temporary pain relief or a loss of sensation from the waist down. An epidural or spinal block can provide complete pain relief during cesarean birth.
An epidural is placed with the woman lying on her side or sitting up in bed with the back rounded to allow more space between the vertebrae. Her back is scrubbed with antiseptic, and a local anesthetic is injected in the skin to numb the site. The needle is inserted between two vertebrae and through the tough tissue in front of the spinal column. A catheter is put in place that allows continuous doses of anesthetic to be given.
This type of anesthesia provides complete pain relief and can help conserve a woman's energy, since she can relax or even sleep during labor. This type of anesthesia does require an IV and fetal monitor. It may be harder for a woman to bear down when it comes time to push, although the amount of anesthesia can be adjusted as this stage nears.
Spinal anesthesia operates on the same principle as epidural anesthesia and is used primarily in cases of c-section delivery. It is administered in the same way as an epidural, but the catheter is not left in place following the surgery. The amount of anesthetic injected is large, since it must be injected at one time. Spinals provide quick and strong anesthesia and allow for major abdominal surgery with almost no pain.
NarcoticsShort-acting narcotics can ease pain and not interfere with a woman's ability to push. However, they can cause sedation, dizziness, nausea, and vomiting. Narcotics cross the placenta and can affect the baby.
Natural childbirth and preparation for childbirth
There are several methods available to prepare for childbirth. The one selected often depends on what is available through the healthcare provider. Overall, family involvement is receiving increased attention by the healthcare systems, and the majority of hospitals now offer birthing rooms and maternity centers to accommodate the entire family.
Lamaze, or Lamaze-Pavlov, is the most commonly used method in the United States as of 2004. It became the first popular natural childbirth method in the 1960s. Various breathing techniques, cleansing breath, panting and blowing, are used for different phases together with the use of a focal point to enable the laboring woman to maintain control. A partner helps by coaching the mother throughout the birthing process.
KEY TERMSAmniotic sac—The membranous sac that contains the fetus and the amniotic fluid during pregnancy.
Breech birth—Birth of a baby bottom-first, instead of the usual head-first delivery. This can add to labor and delivery problems because the baby's bottom doesn't mold a passage through the birth canal as well as does the head.
Cervix—A small, cylindrical structure about an inch or so long and less than an inch around that makes up the lower part and neck of the uterus. The cervix separates the body and cavity of the uterus from the vagina.
Embryo—In humans, the developing individual from the time of implantation to about the end of the second month after conception. From the third month to the point of delivery, the individual is called a fetus.
Gestation—The period from conception to birth, during which the developing fetus is carried in the uterus.
Perineum—The area between the opening of the vagina and the anus in a woman, or the area between the scrotum and the anus in a man.
Placenta—The organ that provides oxygen and nutrition from the mother to the unborn baby during pregnancy. The placenta is attached to the wall of the uterus and leads to the unborn baby via the umbilical cord.
Vertex—The top of the head or highest point of the skull.
The Read method, named for Dr. Grantly Dick-Read (who published his book Childbirth Without Fear in 1944) involves primarily remaining relaxed and breathing normally. Dr. Dick-Read promoted this method in the 1930s to help mothers deal with apprehension and tension associated with childbirth. He emphasized the practice of tensing and relaxing muscles so that complete relaxation occurs between contractions in labor. This action also serves to promote good oxygenation to the muscles.
The Bradley method is called father-coached childbirth, because it focuses on the father serving as the coach throughout the process. It encourages normal activities during the first stages of labor without interventions and focuses on breathing and relaxation.
HypnoBirthing is becoming increasingly popular in the United States in the early 2000s and has proven to be quite effective. Based upon the work of Grantly Dick-Read, it teaches the mother to understand and release the fear-tension-pain syndrome, which so often is the cause of pain and discomfort during labor. When people are afraid, their bodies divert blood and oxygen from non-essential defense organs to large muscle groups in their extremities. Unfortunately, the body considers the uterus to be a non-essential organ. HypnoBirthing explores the myth that pain is a necessary accompaniment to a normal birthing. When a laboring woman's mind is free of fear, the muscles in her body, including her uterine muscles, relax, thus facilitating an easier, stress-free birth. In many cases, first stage labor shortens, which diminishes fatigue during labor leaving the mother stronger for pushing. The founder of HypnoBirthing, Marie Mongan, promotes the philosophy that eliminating fear allows the woman's body to work like it is supposed to.
The LeBoyer method stresses a relaxed delivery in a quiet, dimly lit room. It strives to avoid overstimulation of the baby and to foster mother-child bonding by placing the baby on the mother's abdomen and having the mother massage him or her immediately after the birth. This is followed by the father giving the baby a warm bath.
See also Apgar testing; Electronic fetal monitoring; Cesarean section.
Resources
BOOKSMurkoff, H. I., et al. What to Expect When You're Expecting, 3rd ed. New York: Workman Publishing, 2002.
Olds, Sally, et al. Maternal-Newborn Nursing & Women's Health Care, 7th ed. Saddle River, NJ: Prentice Hall, 2004.
Simkin, Penny, et al. The Labor Progress Handbook. Ann Arbor, MI: Blackwell Publishing, 2000.
Simkin, Penny. Pregnancy, Childbirth, and the Newborn, Revised and Updated: The Complete Guide. Minnetonka, MN: Meadowbrook Press, 2001.
ORGANIZATIONSAmerican Academy of Husband-Coached Childbirth. PO Box 5224, Sherman Oaks, CA 91413–5224. Web site: http://.
Childbirth Enhancement Foundation. 1004 George Avenue, Rockledge, Fl 32955. Web site: http://.
HypnoBirthing Institute. PO Box 810, Epsom, NH 03234. Web site: http://.
International Association of Parents and Professionals for Safe Alternatives in Childbirth. Rte. 1, Box 646, Marble Hill, MO 63764. Web site: http://.
International Childbirth Education Association. PO Box 20048, Minneapolis, MN 55420. Web site: http://.
Lamaze International. 2025 M Street, Suite 800, Washington DC 20036–3309. Web site: http://.
Linda K. Bennington, MSN, CNS